The Connection Between Depression and Chronic Sleep Disorders
Depression and chronic sleep disorders often go hand in hand, and this creates a cycle that is hard to break. Though both can exist independently, they often trigger each other, making their interplay complex in mental and physical health challenges. Understanding this connection is therefore important for effective treatment and recovery.
How Depression and Sleep Disorders Are Linked
1.Shared Biological Mechanisms: Depression and sleep disorders, such as insomnia or hypersomnia, share common imbalances in neurotransmitters like serotonin and dopamine. These chemicals regulate mood and sleep, and the loss of balance can worsen both conditions.
2.Sleep Deprivation as a Trigger: Chronic sleep deprivation can trigger disturbances in mood, including irritability, anxiety, and then depression. Poor sleep quality can eventually prevent the brain from regulating emotions effectively over time.
3.Depression’s Impact on Sleep: Depression often disrupts sleep patterns, causing insomnia, or hypersomnia, excessive sleeping. Both conditions contribute to fatigue and feelings of hopelessness, hallmark symptoms of depression.
4.The Vicious Cycle: Sleep problems can worsen depression, and depression can worsen sleep problems. This bidirectional relationship makes it challenging to determine which condition came first, but addressing both simultaneously is often necessary for improvement.
Breaking the Cycle: Treatment Strategies
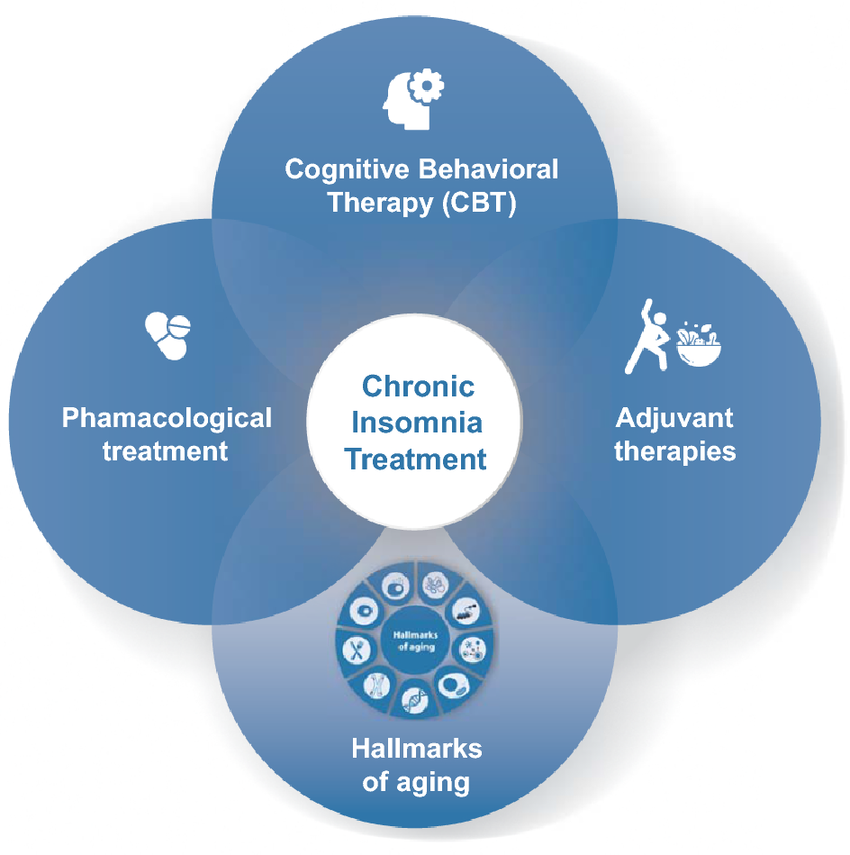
1.Cognitive Behavioral Therapy (CBT):
CBT, CBT-I, specifically has been identified as a successful intervention that will assist in eliminating maladaptive negative thought patterns involved with both depression and sleep.
Additional techniques like stimulus control and education in sleep hygiene will contribute to improved sleep, thereby aiding in improving mood.
2.Lifestyle Changes:
Exercise on a daily basis improves endorphins, helps to diminish depression, and promotes good sleep.
Keeping a regular sleep schedule and establishing a soothing bedtime ritual support healthy sleep habits.
3.Mindfulness and Relaxation Techniques:
Regular practice of meditation, deep breathing exercises, and progressive muscle tension can reduce stress and bring the mind to a relaxing state.
4.Medical Interventions:
Medications that improve serotonin levels may help alleviate the symptoms of depression and disorders related to sleep.
Benzodiazepines in Treatment
Benzodiazepines are sometimes prescribed if severe sleep disturbances and even anxiety due to depression do not respond to other methods of treatment. These drugs function by augmenting the activity of the neurotransmitter GABA, which leads to a calming effect on the brain. Although benzodiazepines can offer short-term help for acute insomnia or anxiety, they are generally not prescribed for long-term treatment because of the possibility of addiction and tolerance. Individuals must, therefore, consult with their healthcare provider to assess the risks versus the benefits before embarking on this therapy. When used judiciously, in conjunction with other forms of therapy, benzodiazepines can certainly be an effective adjunct of a comprehensive treatment plan.
Conclusion
The connection between depression and chronic sleep disorders highlights the importance of treating both conditions simultaneously. Addressing the underlying causes and combining therapy, lifestyle changes, and medical interventions when necessary can break this challenging cycle. Better sleep and improved mental health are achievable goals with the right support.