OCD Beyond Cleanliness: Debunking the Biggest Myths
For most people who hear the word Obsessive-Compulsive Disorder (OCD), what pops into mind is a germophobe washing hands excessively or a neat freak trying to keep everything in pristine order. Cleaning and organization might indeed be facets of OCD, but they do not represent an aspect of the broader scope this mental health issue presents. Unfortunately, pop culture and widespread misconceptions have watered down the concept of OCD to a caricature, thus making it that much more challenging for those in need of a cure.
In reality, it is a very intrusive and often debilitating condition that goes far beyond a simple need for tidiness. It is characterized by obsessions (persistent, unwanted thoughts, fears, or urges) and compulsions (repetitive behaviors or mental rituals performed to reduce anxiety). These compulsions are not about preference or personality quirks—they stem from intense distress and, if left untreated, can take over a person’s daily life.
The myths about OCD do not just cause misunderstandings; rather, they contribute to stigma, the risk of misdiagnosis, and also barriers to treatment. In the next article, we will uncover some of the most widespread myths about OCD and shine light on what is really going on instead. If you, or someone you know, has OCD, knowing the facts is a key first step in dispelling these damaging myths.
Let’s separate fact from fiction and find out what OCD really is.
What is OCD?
OCD is a chronic mental health condition characterized by recurrent, intrusive thoughts (obsessions) and repetitive behaviors or mental rituals (compulsions) performed to reduce anxiety. Obsessions might range from fear of contamination or fear of harm to unwanted taboo thoughts. Compulsions may be excessive checking, counting, seeking reassurance, or similar actions. Contrary to some of the usual misconceptions about OCD, the disorder is certainly not just an obsessive interest in cleanliness or neatness. Indeed, OCD can be a significantly debilitating condition affecting daily life; compulsions offer temporary relief from anxiety but actually tend to contribute to the anxiety cycle, from which individuals become unable to recover without professional therapy, such as CBT, or medication.

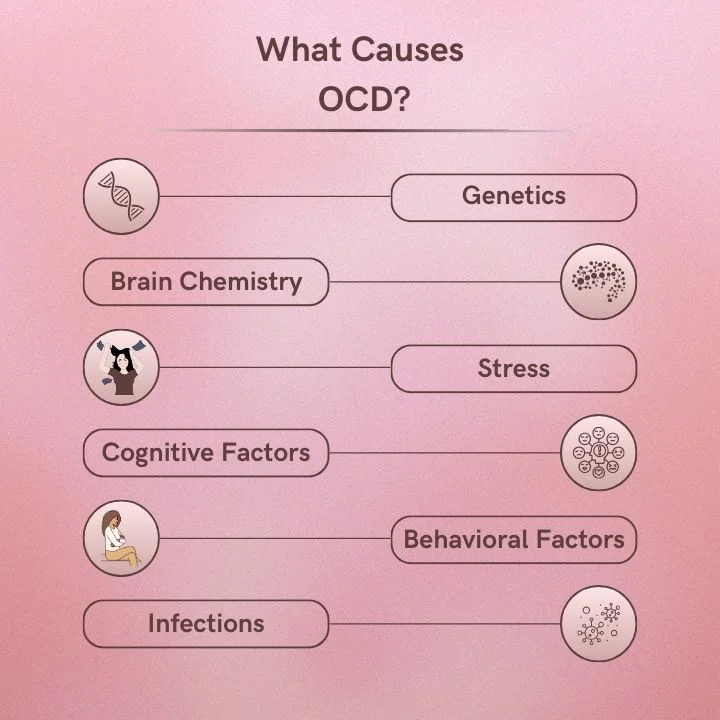
Causes of Obsessive compulsive disorder:
Researchers have not identified the exact cause of Obsessive-Compulsive Disorder (OCD), but they have shown that a combination of biological, psychological, and environmental factors causes it.
a. Genetics : OCD tends to run in families, which indicates a genetic component. Studies suggest that individuals with a close relative who has OCD are at a higher risk of developing the disorder, though specific genes involved are still being studied.
b. Brain structure and function: Research has linked OCD to structural and functional differences in the brain, particularly in areas responsible for decision-making, impulse control, and emotional regulation, such as the orbitofrontal cortex, basal ganglia, and thalamus. Scientists have also implicated neurotransmitter imbalances, especially those involving serotonin.
c. Environmental Triggers : Traumatic life events, childhood trauma, or stress can be some of the reasons for the onset of OCD. Infections such as strep throat have triggered the sudden onset of OCD symptoms in some children. This is sometimes referred to as PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections).
d. Cognitive and Behavioral Factors : Other scientists hypothesize that, in order to neutralize the perceived threat of intrusive thoughts, individuals with OCD may develop maladaptive thought patterns.
While no single factor explains OCD, experts believe a combination of these factors causes the disorder. Fortunately, with the right treatment – such as Cognitive Behavioral Therapy (CBT), Exposure and Response Prevention (ERP), and medication, such as SSRIs – many individuals with OCD can be managed effectively.
Biggest myths about Obsessive compulsive disorder:
Myths and stereotypes often overshadow the true nature of Obsessive-Compulsive Disorder (OCD), leading to misunderstandings. Many people assume OCD is just about being neat or liking things a certain way, but the reality is far more complex. These misconceptions can minimize the struggles of those living with OCD and make it harder for them to seek proper support. Let’s break down the biggest myths and uncover the truth about this often-misrepresented condition.
1. Myth #1: OCD is Just About Cleanliness and Order
One of the most common misconceptions about OCD is that it is solely related to hygiene, tidiness, and an aversion to germs. While some people with OCD do struggle with contamination fears, many others experience completely different types of intrusive thoughts and compulsions.
Reality: OCD Takes Many Forms
Obsessions (persistent, unwanted thoughts, fears, or urges) and compulsions (repetitive behaviors or mental rituals to alleviate distress) define OCD. Some of the lesser-known subtypes of OCD include:
- Harm OCD – Fear of causing harm to oneself or others, even without intent.
- Relationship OCD (ROCD) – Persistent doubts about one’s relationship, partner, or feelings.
- Existential OCD – Obsessive questioning about the meaning of life, reality, or the universe.
- Sex-specific OCD: obsessive thoughts and ruminations around sexual orientation.
- symmetry and order OCD: desires for symmetry that go beyond normal organization.
As these subcategories illustrate, the disorder is certainly not just cleaning; it involves unwanted thoughts creating compulsions. It does not matter what it is about—be it dirty or not.
2. Myth #2: Everyone’s “A Little OCD
How often have you heard someone say, “I’m so OCD about my desk” or “I have OCD when it comes to organizing my closet”? This statement minimizes the serious nature of OCD and misrepresents the actual experience of those living with the disorder.
Reality: OCD is a Serious Mental Health Condition
While many people enjoy organization or have personal preferences for cleanliness, OCD is not just about being neat. It involves crippling anxiety, distress, and time-consuming compulsions that interfere with daily life.
For instance, one with Harm OCD may spend their hours analyzing thought patterns, thinking that they’ll harm someone else. A patient with Contamination OCD may start washing their hands so frequently until the skin may become raw. These experiences reach far beyond preferring to be a neat freak.
3. Myth #3: OCD is Easy to Control With Willpower
People with OCD are often told to “just stop thinking about it” or “ignore the thoughts”, as if it’s a simple matter of willpower. Unfortunately, this advice does not work and can actually make symptoms worse.
Reality: OCD is a Neurological Condition
OCD is associated with the brain’s serotonin system dysfunction and altered activity in the cortico-striato-thalamo-cortical (CSTC) circuit. In other words, it is not a habit or personality quirk but a brain-based disorder that needs proper treatment.
4. Myth #4: OCD is Rare
Many people assume that OCD is an uncommon condition, affecting only a small percentage of the population.
Reality: OCD Affects Millions Worldwide
The World Health Organization states that OCD is one of the top 10 most disabling conditions worldwide. The lives of thousands of people are disarranged due to loss of income and lowered quality of life. It affects about 2-3% of the population, meaning millions of people suffer from it on a daily basis.
5. Myth #5: Avoiding Triggers Can Cure OCD
Some believe that avoiding the things that trigger OCD will help alleviate the disorder. While avoidance might provide short-term relief, it actually reinforces the cycle of anxiety and compulsions.
Reality: Exposure and Response Prevention (ERP) is the Gold Standard for Treatment
The most effective treatment for OCD is Exposure and Response Prevention, a form of Cognitive Behavioral Therapy. ERP gradually exposes the person to feared thoughts or situations and helps them resist compulsions; it teaches the brain that the anxiety will be natural and fade with time, and not require the performance of rituals.

Breaking the Stigma: Understanding the True Nature of OCD
Obsessive-compulsive disorder (OCD) has been reduced to stereotypes for most people, whether having an overcompulsion for cleanliness, perfection, or rigidity. The reality, however, is that OCD is a serious mental illness sometimes medically debilitating, which exceeds all the implications put forth by such stereotypes. OCD is defined through bothersome obsessions, concomitant recurring thoughts or overt compulsions carried out to reduce distress. These compulsions are not based on preference or habit but on an overwhelming need to prevent a feared outcome, even if the individual realizes that their fears may be irrational. Misconceptions about OCD can create stigma, which is a hindrance to people suffering from this disorder in seeking help or feeling understood. Most people with OCD silently suffer from their condition because they fear being judged or dismissed by others.
Breaking the stigma would require a shift in how we talk about and perceive OCD; it is not a personality but a serious condition that can impact every aspect of a person’s life. It is essential to have greater awareness, education, and empathy so that people get proper diagnosis and treatment, including Cognitive Behavioral Therapy (CBT), Exposure and Response Prevention (ERP), and medication when needed. By truly understanding the nature of OCD, we can help promote the kinder, more accurate conversation the disorder so desperately needs-and dispel many myths that have driven out reality for too long.
Conclusion
OCD is much more than a preference for cleanliness or order—it is a serious and often overwhelming mental health condition that affects millions of people worldwide. OCD myths distort public understanding and fuel stigma, making it harder for those suffering to seek help or gain acceptance. Recognizing that intrusive thoughts and compulsions—not quirks or personality traits—drive OCD helps promote a more compassionate and informed perspective.
Education and awareness are key in breaking down these misconceptions and ensuring that individuals with OCD receive the support and treatment they deserve. Whether it is therapy, medication, or other coping strategies, OCD is manageable, and no one should have to suffer in silence. The more we challenge the myths and spread the truth, the closer we come to a world where those with OCD feel understood, validated, and empowered to seek the help they need.